What happens inside our bodies as we commence a new flare up of Diverticulitis.
Diverticulitis is an unpredictable and often painful condition that can disrupt daily life without warning. One moment, you’re feeling fine—eating well, staying hydrated, and managing your gut health. The next, a flare-up strikes, bringing discomfort, cramping, and uncertainty. But what exactly happens inside the body when a flare-up begins? What triggers the transition from a stable gut to painful inflammation? And most importantly—can we detect these early changes before they escalate into a full-blown flare?
At IntelliGut, we are diving deep into the science of diverticulitis to better understand the different stages of a flare-up. By tracking subtle changes in gut activity—through gas patterns, microbial shifts, and physiological markers—we developed an early warning system that alerts users before symptoms become severe.
Here, we’ll break down the progression of a diverticulitis flare-up, from a healthy state to the severe inflammatory stage. Understanding these phases can help sufferers take proactive steps, such as adjusting their diet, increasing hydration, managing stress, or seeking medical attention earlier.
A healthy gut and colon with no Diverticula
Let’s explore what happens inside the gut when diverticulitis takes hold—and how early detection could change the way we manage this condition.
Phase 0: Healthy/Quiescent State
Colon Condition: Diverticula (small pouches in the intestinal wall) are present but not inflamed. These may be asymptomatic.
Symptoms/Indicators: Typically none. Normal bowel movements, no significant pain or discomfort.
Key Characteristics: Stable gut microbiome, normal bowel movements, no inflammation markers elevated.
Goal at This Phase: Maintain stability, detect any subtle shifts before inflammation starts.
A single diverticulum protruding the colon, people with diverticulosis usually have 10 or more diverticulum
In this phase, the colon is functioning normally, and diverticula—small, pouch-like sacs that form in the intestinal wall—are present but not causing any issues. This condition, known as diverticulosis, is common, especially with age, and often remains asymptomatic for many individuals.
Colon Condition:
At this stage, the diverticula are uninflamed and do not disrupt normal digestive processes. The intestinal walls are intact, the gut microbiome is balanced, and the colon is efficiently processing food and waste without complications.
Symptoms & Indicators:
No pain, discomfort, or bloating
Regular and healthy bowel movements
No signs of inflammation or infection
Key Characteristics:
✅ Stable Gut Microbiome – A diverse and balanced population of bacteria supports digestion and protects against harmful pathogens.
✅ Normal Bowel Function – Food moves efficiently through the intestines, and stool is well-formed.
✅ No Immune Response Activation – No elevation in inflammatory markers or immune activity.
Goal at This Phase:
The primary focus in Phase 0 is maintenance and prevention. Since the colon is stable, this is the ideal time to adopt healthy habits—such as maintaining a fiber-rich diet, staying hydrated, and managing stress—to prevent a future flare-up. Additionally, subtle shifts in gut health may occur long before symptoms arise, making early detection crucial for preventing inflammation.
By tracking gut microbiome changes, gas composition, and physiological markers, IntelliGut aims to provide early warnings of any disturbances—helping individuals maintain long-term gut stability and avoid unnecessary flare-ups.
Phase 1: Early Irritation / Pre-Inflammatory Stage
Colon Condition: Some mild irritation within the diverticula. Possibly due to changes in stool composition, minor abrasions, or mild bacterial overgrowth.
Symptoms/Indicators: May be vague or nonexistent. Possibly very mild discomfort, slight changes in bowel habit, minor bloating or subtle cramping.
Biological Markers: Very slight changes in local inflammation markers; possibly normal systemic markers. Microbiome might start shifting.
Goal at This Phase: Detect subtle shifts that usually go unnoticed—changes that precede inflammation.
The individual diverticulum are mildly irritated and red.
In this early stage, the diverticula remain structurally intact, but mild irritation begins to develop. These changes are often subtle and easily overlooked, as they do not yet trigger significant symptoms. However, this is a critical phase where early intervention—such as dietary adjustments or stress management—could help prevent progression to full-blown inflammation.
Colon Condition:
Mild irritation within the diverticula, potentially caused by:
Changes in stool consistency (hard stool pressing against the diverticula).
Minor abrasions from rough or undigested food particles.
Bacterial overgrowth, leading to increased gas production and mild inflammation.
The colon wall is still structurally healthy, but early inflammatory signals may be starting.
Symptoms & Indicators:
Often no noticeable symptoms at all.
Mild bloating, slight cramping, or subtle discomfort (if present).
Changes in bowel habits, such as minor constipation or slight diarrhea.
Biological Markers:
Very early signs of localized inflammation (though systemic inflammation is often undetectable).
Subtle shifts in microbiome composition, with a possible increase in gas-producing bacteria.
Goal at This Phase:
The goal during Phase 1 is early detection—identifying subtle shifts before they escalate into full inflammation. Many people do not recognize this stage because the body compensates well, and discomfort is minimal. However, IntelliGut’s real-time gut tracking aims to detect early warning signals—such as increased gas levels, microbiome imbalances, or minor inflammatory shifts—helping users make proactive adjustments before a flare-up begins.
Phase 2: Low-Grade Inflammation Onset
Colon Condition: Diverticula start showing mild inflammation. The area may become more sensitive and begin producing local inflammatory signals.
Symptoms/Indicators: Mild pain, slight and intermittent. Stool changes in frequency or consistency. Possibly some early fatigue or low-level systemic signals.
Biological Markers: Slight elevation in local inflammatory markers (e.g., calprotectin). Subtle increases in CRP (if tested), or small shifts in heart rate variability due to pain/discomfort.
Goal: Catch at this stage to prompt dietary or stress management interventions, prevent escalation.
The diverticula on the colon are inflamed and slightly painful when pressing hard on the abdomen.
At this stage, inflammation begins to take hold, marking the transition from mild irritation to an early inflammatory response. The diverticula are now slightly inflamed, and the body starts activating localized immune responses to manage the irritation. While this phase may still be mild and manageable, it represents a tipping point—without intervention, inflammation can escalate into a more severe flare-up.
Colon Condition:
Diverticula show early signs of inflammation, with minor swelling and increased sensitivity.
The surrounding intestinal tissue may become irritated, leading to mild cramping and discomfort.
The gut lining may start producing local inflammatory signals, such as cytokines, to respond to stressors.
Symptoms & Indicators:
Mild, intermittent pain (often localized in the lower left abdomen).
Changes in bowel habits—stool may become softer, harder, or vary in frequency.
Possible early signs of fatigue or feeling slightly “off.”
Mild bloating and increased gas production.
Biological Markers:
Slight elevation in local inflammation markers (e.g., calprotectin in stool).
CRP (C-reactive protein) may begin to rise in some individuals (if tested).
Heart rate variability (HRV) may shift slightly due to discomfort or stress.
Goal at This Phase:
Phase 2 is a crucial intervention window—this is where lifestyle changes can still prevent escalation into a painful, full-blown flare-up. At this stage, IntelliGut’s tracking system would detect:
Inflammation markers increasing before systemic inflammation takes hold.
Changes in gut gas composition that indicate microbial shifts.
HRV and stress fluctuations, which can be linked to digestive function.
With early detection, users can take preventative actions such as adjusting fiber intake, increasing hydration, reducing stress, and monitoring triggers—potentially stopping a flare-up before it worsens.
Phase 3: Moderate Inflammation / Pre-Flare
Colon Condition: Inflammation is more pronounced. The colon wall is irritated; immune cells are more active in the area. Potential beginning of mucosal swelling.
Symptoms/Indicators: Noticeable consistent pain or tenderness in a localized area (often lower left quadrant), more frequent bloating, altered bowel patterns (constipation or diarrhea), mild systemic signs like low-grade fever or feeling “off.”
Biological Markers: Elevated fecal calprotectin, CRP may be mildly elevated. Possibly detectable changes in the microbiome composition.
Goal: Definitely intervene here with dietary changes, possibly mild medication, increased hydration, rest, or other doctor-advised strategies.
The inflamation is getting worse and the lower abdomen in painful.
At this stage, inflammation is no longer subtle—the immune system is actively responding, and the colon wall is becoming increasingly irritated. The body is signaling that something is wrong, and discomfort becomes more persistent and noticeable. This is a critical intervention point, where targeted dietary, lifestyle, and medical strategies can help prevent full escalation into an acute flare-up.
Colon Condition:
Inflammation is more pronounced, affecting the diverticula and surrounding colon tissue.
The immune system is more active, sending white blood cells and inflammatory cytokines to the affected area.
The colon wall may begin to swell, leading to mild narrowing of the intestinal passage.
Mucosal irritation increases, possibly triggering more gas, bloating, and irregular stool patterns.
Symptoms & Indicators:
Consistent, localized pain or tenderness, often in the lower left abdomen.
More frequent bloating and increased gas production.
Altered bowel patterns, including periods of constipation or diarrhea.
Mild systemic signs such as a low-grade fever, fatigue, or feeling “off.”
Biological Markers:
Elevated fecal calprotectin (a marker of intestinal inflammation).
CRP (C-reactive protein) may be mildly elevated, indicating a growing inflammatory response.
Changes in microbiome composition, with a shift towards bacteria linked to inflammation.
Goal at This Phase:
At Phase 3, intervention is no longer optional—this is the point where deliberate action is needed to stop progression into a full-blown diverticulitis flare. Key actions include:
✔ Dietary adjustments (reducing fiber or opting for an easily digestible diet).
✔ Hydration and gut rest to reduce colon irritation.
✔ Mild medication (such as anti-inflammatory or gut-soothing agents) if advised by a doctor.
✔ Reducing stress and monitoring symptoms closely.
At this stage, IntelliGut’s data tracking would detect significant shifts in gut gas composition, microbiome changes, and inflammatory markers, providing timely alerts that allow users to take immediate action before the condition worsens.
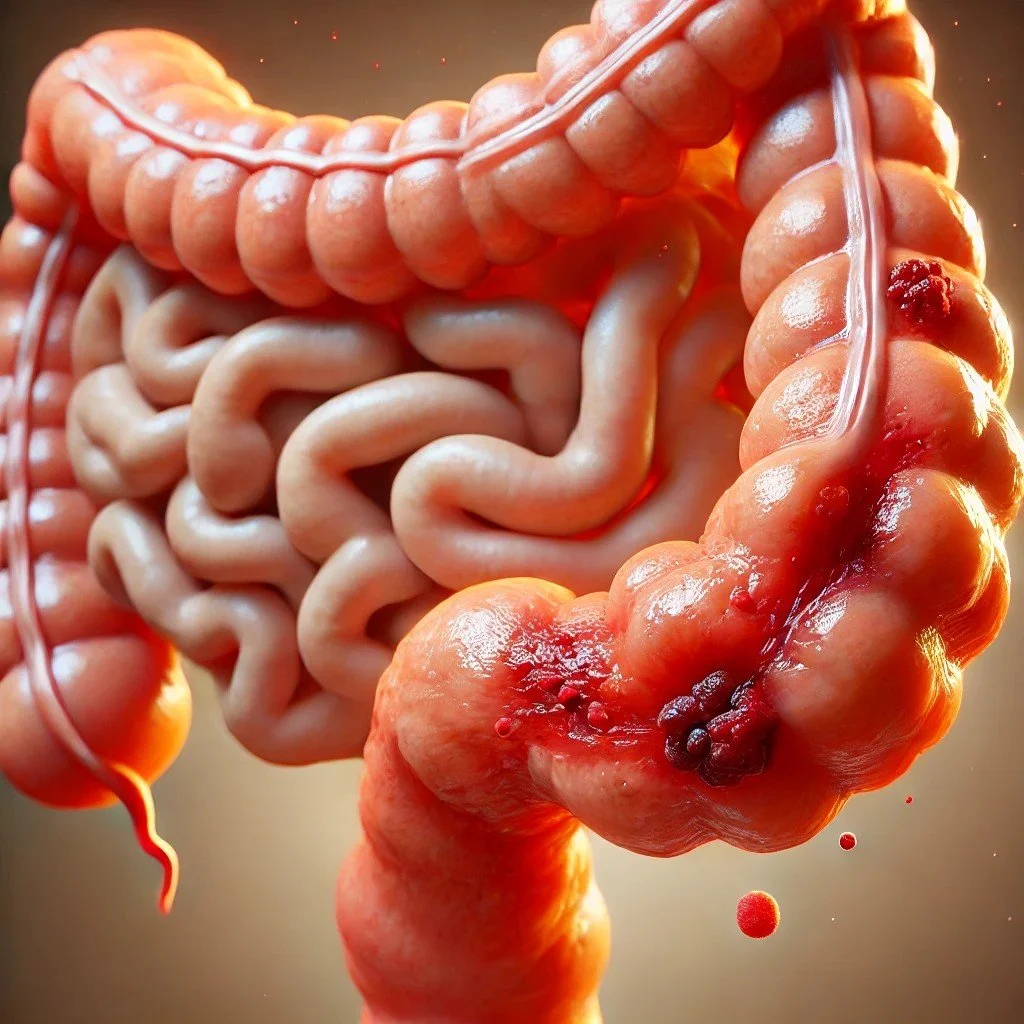
Phase 4: Acute Flare-Up
Colon Condition: Active inflammation and possibly beginning of infection in the diverticula. There’s edema, potential micro-perforations, and a higher bacterial load.
Symptoms/Indicators: Significant pain, tenderness, sometimes fever, nausea. Pronounced changes in bowel habits, possibly blood in stool.
Biological Markers: High fecal calprotectin, elevated CRP, white blood cell count elevated.
Goal: Urgent treatment, often antibiotics, clear liquid diet, and medical supervision to prevent complications or hospitalization.
The diverticula are infected and very painful.
At this stage, inflammation has fully taken hold, and the body is now actively fighting what it perceives as an infection or injury. The diverticula are not just irritated—they may be harboring excess bacteria, triggering an intense immune response. This can lead to painful swelling, localized infection, and in severe cases, the beginnings of micro-perforations in the colon wall.
This is a high-risk phase where intervention is no longer optional—urgent treatment is required to prevent further complications, such as an abscess, perforation, or sepsis.
Colon Condition:
Active inflammation in the diverticula and surrounding colon tissue.
Edema (swelling) in the intestinal wall, possibly narrowing the passageway and making digestion painful.
A significant increase in bacterial activity, as immune cells attempt to neutralize potential infection.
Risk of micro-perforations, which could lead to the spread of bacteria beyond the intestine.
Symptoms & Indicators:
Severe, persistent pain and tenderness, typically in the lower left abdomen.
Bowel habits drastically change—diarrhea, constipation, or alternating between both.
Fever and chills, as the body’s immune system works to control infection.
Nausea, loss of appetite, and fatigue due to the systemic inflammatory response.
Possible blood in stool, signaling irritation or minor bleeding within the colon.
Biological Markers:
High fecal calprotectin, indicating severe inflammation in the gut.
Elevated CRP (C-reactive protein) and white blood cell count, confirming an active inflammatory or infectious process.
Goal at This Phase:
At Phase 4, immediate treatment is required. Medical supervision is strongly advised, and common interventions include:
✔ Antibiotics to control bacterial overgrowth and infection risk.
✔ Clear liquid diet or bowel rest to allow the gut to heal.
✔ Pain management and anti-inflammatory medications (under medical supervision).
✔ Close monitoring for worsening symptoms—if pain becomes unbearable or fever spikes, hospitalization may be necessary.
At this stage, IntelliGut’s advanced tracking system would detect major changes in gut gas composition, inflammatory markers, and systemic signals, providing urgent warnings that help users recognize when they need immediate medical attention.
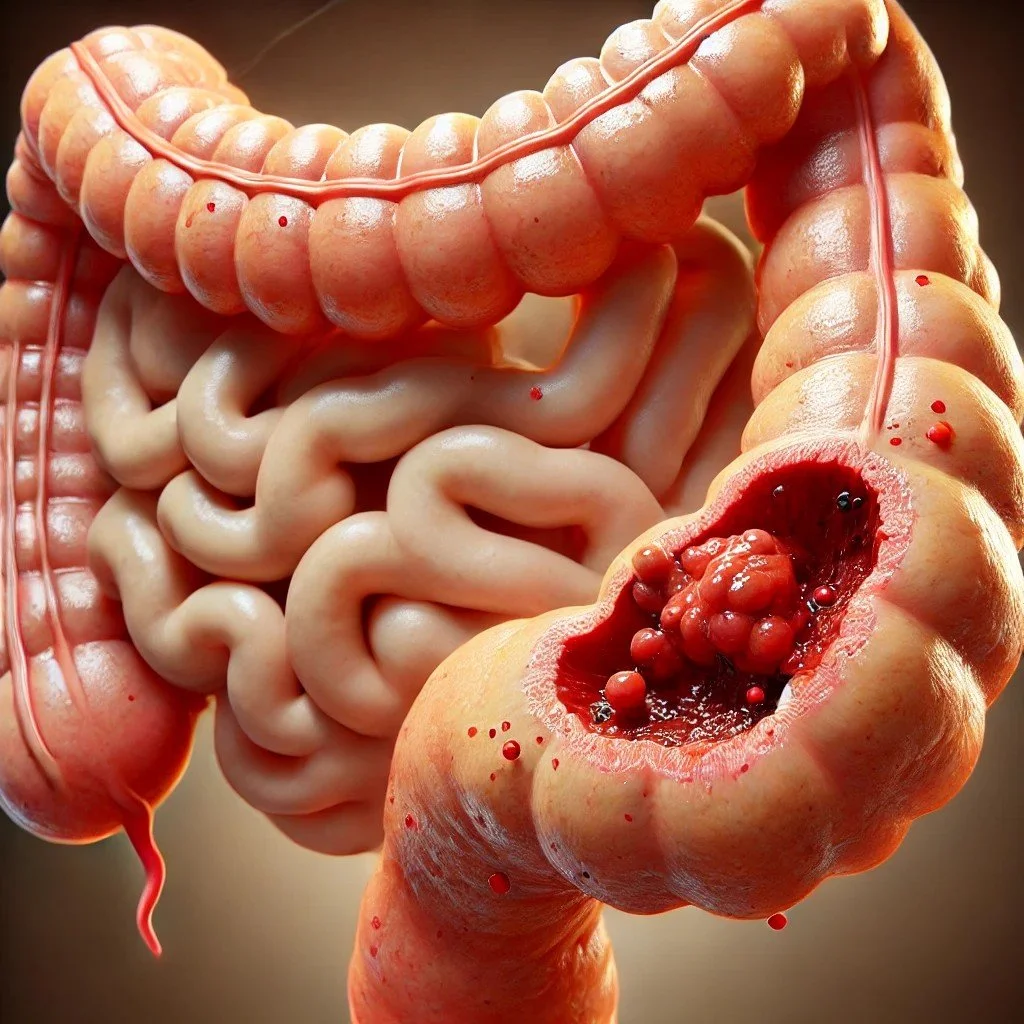
Phase 5: Severe Flare / Complications
Colon Condition: If untreated, can lead to severe infection, abscess formation, perforation, peritonitis.
Symptoms/Indicators: Severe abdominal pain, high fever, severe changes in vital signs, possibly emergency situation.
Biological Markers: Markedly high inflammatory markers, imaging abnormalities on CT scan or ultrasound.
Goal: Immediate medical intervention—hospitalization, IV antibiotics, possibly surgery.
Diverticulitis has progressed to a critical state where a severe infection poses a serious health risk.
At this stage, diverticulitis has progressed to a critical state, where severe inflammation, infection, or structural damage poses a serious health risk. The body is no longer able to contain the inflammatory response, and complications such as abscesses, perforations, or peritonitis (infection of the abdominal cavity) may develop.
This phase is a medical emergency requiring immediate hospitalization to prevent life-threatening complications.
Colon Condition:
Severe infection and inflammation, with the potential for bacterial spread beyond the intestine.
Risk of abscess formation, where infected fluid collects in pockets near the colon.
Potential perforation (rupture) of the colon wall, allowing bacteria to leak into the abdominal cavity.
Peritonitis (a dangerous, widespread abdominal infection) if bacteria enter the peritoneal lining.
Symptoms & Indicators:
Severe, unrelenting abdominal pain, often worsening with movement.
High fever and chills, indicating a systemic infection.
Severe changes in vital signs, including rapid heart rate, low blood pressure, and signs of shock.
Nausea, vomiting, and inability to pass stool, suggesting a blockage or worsening inflammation.
Biological Markers:
Markedly high inflammatory markers, including CRP and white blood cell count.
Elevated fecal calprotectin, confirming extensive intestinal inflammation.
Imaging abnormalities on CT scan or ultrasound, revealing abscesses, thickened colon walls, or perforations.
Goal at This Phase:
This is an emergency situation, and immediate medical intervention is required. Hospitalization is necessary, with treatment options including:
✔ IV antibiotics to control systemic infection.
✔ Fluid resuscitation and close monitoring of vital signs.
✔ Surgical intervention, such as drainage of an abscess or, in severe cases, bowel resection surgery to remove damaged sections of the colon.
At Phase 5, IntelliGut’s real-time tracking would have detected progressive worsening over earlier stages, allowing for early intervention before reaching this point. However, for those experiencing sudden deterioration, IntelliGut could still provide urgent alerts based on key physiological data—prompting users to seek immediate emergency care.